Relationship between Endometrial Thickness and Pregnancy Outcomes in Assisted Reproductive Technology Cycles
Relationship between Endometrial Thickness and Pregnancy Outcomes in Assisted Reproductive Technology Cycles
DOI:
https://doi.org/10.69614/ejrh.v15i2.667Keywords:
Key Words: assisted reproductive technology, controlled ovarian stimulation, in vitro fertilization, intracytoplasmic sperm injection, endometrial thickness, embryo transferAbstract
ABSTRACT
Objective: To explore the relations of different ultrasonic endometrial thickness (EMT)values on hCG trigger day and the pregnancy rate (PR) after fresh embryo transfer (ET) in controlled ovarian stimulation (COS) cycles.
Background: Successful implantation and delivery require both the functional embryo and receptive endometrium in assisted reproductive technology (ART) cycles which is an expensive procedure with low implantation and pregnancy rate (PR). It is estimated that embryos account for one-third, and suboptimal endometrial receptivity for the remaining two-thirds of implantation failures. There is still an ongoing debate regarding the predictive ability of ultrasonic endometrial evaluation on the day of human chorionic gonadotrophin (hCG) trigger during controlled ovarian stimulation (COS) on the outcomes of pregnancies after in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI).
Method: A retrospective review of data from medical records of all patients who underwent COS, oocyte retrieval, IVF/ICSI, and fresh ET between March 2021and July 2022 at Centre for Fertility and Reproductive Medicine (CFRM), St Paul Millennium medical College (SPHMMC) Addis Ababa, Ethiopia. Patients were categorized based on their ET outcome (as pregnant or non-pregnant) and EMT values on the day hCG trigger (groups A <8mm, B 8-12mm, and C>12 in mm) to study and analyze if any relation between endometrial thickness and pregnancy rate existed.
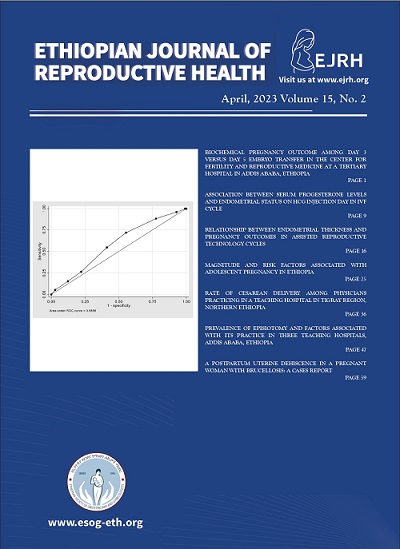
Results: A total of 548 records were analyzed. PR was 40.9%. The odds of pregnancy were higher among patients with EMT group B (82.8% vs 74.6%, p=0.05) and was shown to be significant after controlling for the effects of multiple confounding factors. Although receiver operator curve (ROC) analysis indicated that EMT has a limited value to be used as an indicator of the pregnancy rate as evidenced by the area under the curve (AUC) of 0.59 (95% CI= 0.53, 0.63), it was not possible to determine a cutoff of the endometrial thickness value with an acceptable trade-off between sensitivity and specificity
Conclusion: There is a positive relationship between the EMT measured on the day of hCG injection and PR and that EMT is an independent factor. Further prospective study is needed to explore the issue in more detail in our setup.
References
2. Bu Z, Sun Y. The impact of endometrial thickness on the day of human chorionic gonadotrophin (hCG) administration on ongoing pregnancy rate in patients with different ovarian response. PLoS One. 2015 Dec 1;10(12).
3. Shakerian B, Turkgeldi E, Yildiz S, Keles I, Ata B. Endometrial thickness is not predictive for live birth after embryo transfer, even without a cutoff. Fertil Steril [Internet]. 2021;116(1):130–7. Available from: https://doi.org/10.1016/j.fertnstert.2021.02.041
4. Al-Ghamdi A, Coskun S, Al-Hassan S, Al-Rejjal R, Awartani K. The correlation between endometrial thickness and outcome of in vitro fertilization and embryo transfer (IVF-ET) outcome. Reprod Biol Endocrinol. 2008 Sep 2;6.
5. Yuan X, Saravelos SH, Wang Q, Xu Y, Li TC, Zhou C. Endometrial thickness as a predictor of pregnancy outcomes in 10787 fresh IVF–ICSI cycles. Reprod Biomed Online [Internet]. 2016;33(2):197–205. Available from: http://dx.doi.org/10.1016/j.rbmo.2016.05.002
6. Yang W, Zhang T, Li Z, Ren X, Huang B, Zhu G, et al. Combined analysis of endometrial thickness and pattern in predicting clinical outcomes of frozen embryo transfer cycles with morphological good-quality blastocyst: A retrospective cohort study. Medicine (Baltimore) [Internet]. 2018 Jan 1 [cited 2022 Mar 12];97(2). Available from: /pmc/articles/PMC5943888/
7. Richter KS, Bugge KR, Bromer JG, Levy MJ. Relationship between endometrial thickness and embryo implantation, based on 1,294 cycles of in vitro fertilization with transfer of two blastocyst-stage embryos. Fertil Steril. 2007 Jan;87(1):53–9.
8. Chan JM, Sukumar AI, Ramalingam M, Ranbir Singh SS, Abdullah MF. The impact of endometrial thickness (EMT) on the day of human chorionic gonadotropin (hCG) administration on pregnancy outcomes: a 5-year retrospective cohort analysis in Malaysia. Fertil Res Pr. 2018;4(1):1–9.
9. Dietterich C, Check JH, Choe JK, Nazari A, Lurie D. Increased endometrial thickness on the day of human chorionic gonadotropin injection does not adversely affect pregnancy or implantation rates following in vitro fertilization-embryo transfer.
10. Quintero RB, Sharara FI, Milki AA. Successful pregnancies in the setting of exaggerated endometrial thickness.
11. Wu Y, Gao X, Lu X, Xi J, Jiang S, Sun Y, et al. Endometrial thickness affects the outcome of in vitro fertilization and embryo transfer in normal responders after GnRH antagonist administration. Reprod Biol Endocrinol. 2014 Oct 9;12(1).